Introduction:
It is common for pregnant women to have high blood sugar levels. To put it simply, this is the fundamental definition of gestational diabetes. Gestational or pregnancy diabetes develops during your pregnancy.
However, there is some encouraging news about gestational diabetes. That is, it usually goes away after giving birth to the baby.
Women frequently fail to fully recover from gestational diabetes. Their blood glucose levels will stay somewhat elevated. In some circumstances, it is discovered that such a girl develops diabetes a few years or decades later.
The patient may develop type-2 diabetes, which can be managed with Diabetrol SR.
The advantage is that it can be checked. Yes, you can reverse your high blood sugar levels by implementing some healthy lifestyle changes. One aspect of this diet cannot be overlooked.
So, let’s look at the diet you should follow following gestational diabetes. But first, let’s look at some of the risk factors that lead to gestational diabetes. This will offer you an idea of how to prevent experiencing the same thing during your pregnancy.
What Is Gestational Diabetes?
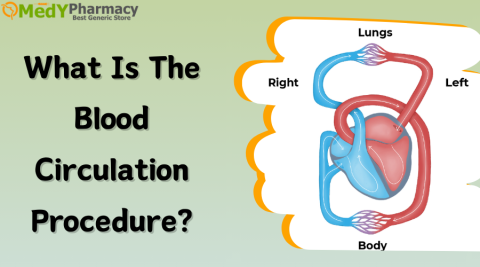
Gestational diabetes occurs during pregnancy. This type of diabetes happens when the body fails to create enough insulin during pregnancy. The pancreas secretes insulin, which allows the body’s cells to use blood sugar for energy.
Pregnancy causes the body to create extra hormones, which can cause weight gain. These alterations can cause cells to use insulin less efficiently than previously, a condition known as insulin resistance.
High blood sugar levels can occur if the pancreas fails to produce enough insulin to keep up. Can be harmful to both the pregnant lady and the unborn child.
Insulin resistance has been linked to pre-pregnancy weight gain and inactivity.
- Tiredness
- Nausea
- Having Exceptional Thirst.
- Urinating Frequently
- Recurrent Bladder Infections
- Blurry Vision
- Sugar in the Urine That Is Identifiable By Testing
When Does Gestational Diabetes Appear During Pregnancy?
Gestational diabetes often develops near the end of the second trimester, between the 24th and 28th weeks of pregnancy. As a precaution, your dialectologist will most likely do a gestational diabetes test at the end of the second trimester.
If left untreated or misdiagnosed, increases your child’s risk of acquiring diabetes in the future. So it is preferable to treat it early on to reduce the risk and difficulties associated with gestational diabetes during pregnancy and delivery.
In these circumstances, a gestational diabetic diet advised by a nutritionist can substantially aid in regulating the mother’s blood sugar levels while also protecting the baby.
How Does Gestational Diabetes Influence The Baby?
In this chapter, we will look at some of the issues associated with gestational diabetes and how they affect the infant. Complications can harm the developing baby, which is why a quick diagnosis is critical to helping reduce their effects throughout the pregnancy. Both the expectant mother and her baby can develop difficulties from gestational diabetes.
- Higher Than Usual Birth Weight
High blood sugar levels during pregnancy can cause their babies to grow larger than usual. This is one type of pregnancy diabetes complication that might result in birth trauma or an emergency C-section delivery because the baby is less likely or unable to pass smoothly through the birth canal.
- Premature Birth
This is closely related to a greater birth weight, in which the woman is obliged to deliver before her due date due to the baby’s huge size.
- Breathing Problems
A dangerous consequence of gestational diabetes is that newborns may have respiratory distress syndrome, a critical condition that impairs breathing.
- Low blood sugar levels
Although gestational diabetes is associated with high blood sugar levels, some infants may experience the opposite shortly after birth. Babies who have extremely low blood sugar levels may experience frequent seizures. However, regulated feeding sessions and intermittent intravenous glucose solutions can be utilized to address low blood sugar levels during birth.
- Future Obesity
Babies born to moms with gestational diabetes are more likely to acquire obesity and type 2 diabetes later in life.
- Stillbirth
Untreated and unmonitored gestational diabetes throughout pregnancy may result in the infant’s death before or shortly after birth.
Gestational Diabetes Treatment using Indian Foods
Above all, prioritize your health when pregnant. A skilled nutritionist can provide useful insights into your nutritional requirements. If you are diagnosed with gestational diabetes, working with a dietitian can help you manage your blood sugar levels efficiently.
Don’t be stressed out by the abundance of information available; instead, focus on self-care and obtaining expert guidance when necessary.
Pregnant women with diabetes can protect themselves and their newborns by closely following a diabetic diet. It can help to avoid the condition’s negative effects and guarantee a smooth pregnancy with a healthy newborn.
- Carbohydrates
These are the most important macronutrients for patients with gestational diabetes. Carbohydrate digestion and absorption can have a major impact on blood glucose levels. Carbohydrate consumption must be monitored to avoid postprandial hyperglycemia.
If you want to control your gestational diabetes with a balanced diet, you can include a variety of carb-rich items in your meals.
- Fruits
Lemon, orange, guava, and green apple can help you achieve your daily vitamin C requirements. These fruits are also a healthy option for satisfying your sweet needs.
- Brown Rice
Brown rice is an excellent replacement for white rice. It has a reduced glycemic index and higher levels of vitamins, minerals, and antioxidants. As part of a well-balanced gestational diabetic diet, moderate brown rice is a good choice for lunch or dinner.
- Grain, Vegetable, And Legumes
Including a range of vegetables like beans, peas, lentils, corn, spinach, and lettuce, as well as whole-grain cereals such as oats, millet, barley, quinoa, and sorghum, will help regulate blood sugar while also providing necessary sustenance for pregnancy health.
These meals are high in fiber and low in glycemic index, which helps your digestive system function properly and reduces your risk of acquiring obesity and type 2 diabetes in the future. Vegetables, grains, and legumes can help both you and your baby with gestational diabetes.
- Protein
Throughout pregnancy, a larger protein intake is required since it plays an important role in the development of maternal components such as the blood, uterus, and breasts, as well as the development of fetal and placental tissues.
- Dry beans, lentils
Red China, rajma beans, chickpeas, and brown, green, and red lentils can all aid with gestational diabetes by supplying essential nutrients including fiber, folate, and iron. These nutrients help treat gestational diabetes.
- Paneer with Soy Chunks
Paneer and soy are two nutrient-dense foods that are widely consumed throughout the world. Aside from being tasty, these foods have various well-documented health benefits. Paneer, for example, is well-known for its weight loss, bone health, and diabetes treatment benefits.
Soy, on the other hand, is high in flavones, a type of molecule that has been associated with a lower risk of diabetes and heart disease. So, to improve your health, incorporate paneer and soy into your gestational diabetes diet.
- Eggs
If you want a diabetes-friendly diet with some delectable options, try to include eggs in your meals. Despite being a non-vegetarian dish, they are low in carbohydrates and can be an excellent addition to your gestational diabetes regimen.
If you’re looking for a nutritious and full dietary option, eggs are worth considering. Remember that, while egg whites provide more protein, yolks include healthy fats that will not spike your blood sugar.
Furthermore, due to their low glycemic index, eggs are an excellent alternative for people who want to avoid quick blood sugar spikes.
- Fish
Consider the nutritional value of fish and seafood. These aquatic treats are high in protein but low in fat.
Furthermore, they are high in omega-3 fatty acids, which help with cognitive function and brain health, particularly in pregnant women.
Beneficial Fats
If you are pregnant and have been diagnosed with gestational diabetes, you should reduce your fat intake. Limit your intake of butter, margarine, salad dressing, cooking oil, and sugary foods.
It is also recommended that you avoid foods high in saturated fat, such as cheese, bacon, and hamburger.
You mustn’t exclude fats and oils from your diet. Select healthy oils such as olive and peanut.
- Avocado
If you’re looking for a nutritious snack, consider a delectable fruit with beneficial fats and vitamins. It has little complex carbs and a low glycemic index. Furthermore, this fruit has been demonstrated to have satiating properties, helping people to feel full for longer periods without consuming too many calories.
- Nuts
Almonds, walnuts, and peanuts are high in critical elements like proteins and healthy fats that enhance heart health. Nuts are an excellent snack for people with gestational diabetes because they include low carbohydrate content and high levels of protein, fiber, and healthy fats, all of which are essential for maintaining a balanced diet.
Identifying the Causes and Risks of Gestational Diabetes
Scientists are still unsure how gestational diabetes occurs. However, the majority believe there are causes. Let’s have a look at some risk factors for developing this condition.
- Increased Weight
During pregnancy, your weight will surely increase by several pounds. According to a comprehensive study, women can gain between 11 and 16 kg during this time. The majority of scientists agree that the overweight issue is to blame.
- Low levels of physical activity
Most women relax a lot during their pregnancy. Of course, women are not permitted to perform any physical labor. However, if you avoid physical activity such as a morning walk, stationed bike ride, or yoga, your blood sugar levels will continue to climb.
- Having Prediabetes Already
If you have pre-diabetes, you are more likely to acquire the disease. With this condition, a lady would have to manage her nutrition, exercise more, and be more cautious than other expectant mothers.
- Eating too much
Most researchers assume that diabetic issues arise during pregnancy as women’s nutritional habits change. During this time, hormonal changes occur, which cause you to feel hungry. Without control over your food choices, you end up eating things that are high in sugar. This is why sugar levels grow dramatically in a matter of months.
- Diet Following Gestational Diabetes
The mother’s blood sugar levels usually recover to normal within a few days or weeks of delivery.
Maintaining such high blood sugar levels over an extended period puts your health at risk.
- Consume zero-sugar products
The simplest and most effective way to reduce sugar is to avoid foods with high sugar content. Find out which foods have a high glycemic index and will produce a sugar spike, then avoid them.
So, what are your eating options here? Spinach, kale, beetroot, and cauliflower and its variations are also options.
What Effects Does Gestational Diabetes Have on the Mother?
While we have seen how gestational diabetes can harm the fetus, it can also impair the pregnant woman.
- High blood pressure
Mothers with gestational diabetes are more likely to have high blood pressure and preeclampsia. Pre-eclampsia is a pregnancy condition that usually appears during the 20th week or even after birth. If left untreated, it can lead to high blood pressure, headaches, blurred vision, protein in the urine, fluid retention, and organ damage, endangering both the mother and the baby’s life.
This may cause growth difficulties in the child as it grows. Although the origins of pre-eclampsia are unknown, they are typically associated with placental issues.
- Delivery by C Section
While not a consequence of gestational diabetes, moms with gestational diabetes are more likely to have a C-section delivery than a normal vaginal delivery.
- Diabetes later in life
A history of gestational diabetes can cause the mother to get the illness again during a subsequent pregnancy. There is also a chance of developing type 2 diabetes in the future.
What Are The Causes Of Gestational Diabetes?
Unfortunately, no one knows exactly what causes gestational diabetes. However, it is assumed that a woman’s endocrine system is involved in the cause. However, we now know that the cause of gestational diabetes is not a lack of insulin, but rather the production of numerous other hormones during pregnancy, which reduces insulin efficacy in the body.
As early as conception, the body begins to create enormous levels of certain pregnancy hormones, which aid in the growth of the baby.
It must transport blood glucose to cells, where it is transformed into energy. It is typical to experience some insulin resistance during pregnancy since glucose in the blood is passed on to the baby. Increased insulin resistance, on the other hand, can produce an unexpected spike in blood glucose levels, resulting in gestational diabetes.
What Are The Symptoms And Indications Of Gestational Diabetes?
Many pregnant women show no uncommon symptoms or indicators of gestational diabetes. Gynecologists commonly administer a gestational diabetes test at the end of the second trimester to determine whether the problem exists or not.
On the other hand, some pregnant women may experience minor symptoms that resemble other types of diabetes.
- Increased thirst
- Fatigue
- Dryness in mouth
- Excessive urination
- Blurred vision
Avoid Overeating And Instead Eat Small, Frequent Meals.
Most studies show that after gestational diabetes, your body experiences sugar increases. To avoid these situations, you must take a decisive move to change your diet.
For example, you can avoid eating a large meal at once. Consuming too much food at once can result in a sugar spike. This is related to consuming a large number of calories all at once in one meal. Instead, a wise strategy is to eat less food per meal while increasing the number of meals.
Food to Limit
Without a doubt, you should avoid sweet sweets, ice cream, fried foods, and red meat. Consuming excessive cholesterol and fats is not an innovative notion when one has high blood sugar.
Avoid milk as well, as studies have shown that it can cause a sugar rise. Some doctors may also advise you to avoid fruits.
Yes, fruits such as bananas, grapes, and mangoes are very sweet. We ask that you avoid it because of its sugar content. Avocadoes, oranges, and berries are all options.
Nutrients to Take
Let us now tell you about the nutrients that are beneficial for sugar regulation. Of course, you should avoid eating fat and cholesterol. Some scientists believe that eating too much protein is also a risk factor.
They believe that consuming a lot of protein causes sugar levels to rise. So, consume protein, but not in excess.
A clever approach is to consume more roughage and fiber. These aid in sugar management. Do not underestimate the importance of vitamins. Some vitamins aid in the absorption of sugar, keeping it from remaining in the bloodstream. Minerals, micronutrients, and flavonoids are the most beneficial to ingest at this time.
Sample Gestational Diabetes Meal Plan
Gestational diabetes does not have to limit your everyday food selection. We’ve created four nutritious and tasty meal plans just for you. To suit your taste, you can try different modifications and combinations of these meal plans. You can find a more thorough diabetes diet chart.
However, it is critical to note that a tailored meal plan recommended by your healthcare professional or dietician is the most effective strategy to control your GD.
What Should I Eat if I Have Gestational Diabetes?
Because refined grains such as white pasta, white rice, white bread, crackers, and tortillas spike blood sugar faster than whole grains, choose whole grains more frequently. The same is true for simple carbohydrates such as sweet desserts and drinks; choose fruit-forward desserts with less added sugar and more fiber. Also, pick entire pieces of fruit over juice.
However, if you want that cookie or brownie, limit yourself to one serving and plan to move around afterward to help your body burn off the sugar. In addition, to general healthy dietary guidelines, avoid fats, choose lean meat or plant-based proteins, and limit processed meals to keep sodium under control.
Complications of Gestational Diabetes
Gestational diabetes raises the possibility of difficulties for both the pregnant woman and the infant.
- Difficulty during labor
- Cesarean delivery
- Heavy bleeding following delivery
- Severe rips in or around the vagina
- A preterm birth
- Having low blood sugar
- Developing type 2 diabetes in later life.
Maintaining a healthy body weight and controlling blood sugar levels after birth can help reduce this risk.
Other Methods of Managing Sugar after Gestational Diabetes
Diet is important for blood sugar regulation. However, there are alternative options for controlling it. Exercise is the second most important aspect of this situation. Regular exercise, yoga, meditation, easy stretching, and amusing hobbies are the best ways to boost metabolism.
Last Words:
Your diet should change dramatically after gestational diabetes for a variety of reasons. Otherwise, you may be left with slightly high blood sugar, which can lead to diabetes later in life.
A dietitian may be able to provide more specialized healthy eating advice for gestational diabetes. Visit Medypharmacy to discover a nutritionist in your area.