Introduction:
Even men can have this condition, however, it is more prevalent in women and affects their reproductive systems and organs. Pelvis The pelvic region is the area between your genitals and your groin.
Prostatitis is the term for pelvic discomfort that can affect men. This kind of pelvic discomfort can be brought on by urinary tract infections, digestive issues, and other male sexual and reproductive illnesses including erectile dysfunction, which requires the usage of medications like Vigora 100.
It is necessary to seek medical advice if you have persistent pelvic pain. We will go into further detail about this man’s pelvic inflammatory illness in this post. This disorder’s causes, symptoms, and available treatments will be investigated.
This illness affects the reproductive organs of women. It usually happens when bacteria from sexual activity move from your vagina to your ovaries, fallopian tubes, or uterus.
One or more higher reproductive organs, such as the ovaries, fallopian tubes, or uterus, are infected. The reproductive tract may develop scar tissue and pockets of contaminated fluid if treatment is not received, which might result in irreversible harm.
This might present with moderate or inconspicuous symptoms and indicators. Some ladies don’t exhibit any symptoms at all. Therefore, it may go undiagnosed until you have chronic pelvic discomfort or difficulty becoming pregnant.
You can have this infection in your ovaries, fallopian tubes, or uterus. Usually, sexually transmitted illnesses are the reason. Vaginal discharge and stomach and lower abdominal aches are among the symptoms. Infertility and other issues can be prevented with prompt PID treatment, which often involves antibiotics. You should also get your spouse checked and treated.
What Is Pelvic Inflammatory Disease?
This infection in your ovaries, fallopian tubes, or uterus is severe. PID arises from the passage of certain germs from the vagina to the reproductive organs. The most frequent cause of PID is bacteria from untreated STIs as well. PID, however, can also be brought on by germs that are often present in the vagina.
This patient may have pelvic or lower abdominal discomfort. A strange discharge from your vagina may also be present. Severe PID can make it impossible for you to conceive and harm your reproductive organs permanently. The most effective method of preventing PID is to get tested and treated for STIs.
The female reproductive system is inflamed in this condition. The most common cause is an untreated, spreading infection in the cervix or vagina.
The uterus, or womb, the fallopian tubes, the ovaries, or a combination of these may be affected. It may cause fibrous bands to grow between tissues and organs, forming scars.
The female reproductive system, which includes the ovaries, fallopian tubes, and uterus, is infected. It often happens when germs contaminate the reproductive organs, frequently from STIs like gonorrhea or chlamydia.
- Pelvic discomfort
- Abnormal vaginal flow
- Painful intercourse
- An irregular menstrual flow
- Cooling and fever
- Urinating painfully
Serious side effects include infertility, persistent pelvic discomfort, and ectopic pregnancy may result if treatment is not received.
To treat the infection, antibiotics are usually used; in more serious situations, surgery or hospitalization may be required. To avoid long-term problems, early treatment is crucial. Safe sex practices and routine STI tests can help lower the incidence of PID.
Risk Factors for Pelvic Inflammatory Disease
You are more likely to develop pelvic inflammatory disease if you have chlamydia, gonorrhea, or a history of STIs. But you can have PID without ever getting an STI.
- Sexing someone younger than 25
- Have several sexual partners
- Intercourse without a condom
- Recently receiving a douching intrauterine device (IUD)
Multiple sexual partners are more likely to be exposed to STIs, which elevates the risk of PID. PID can result from STIs, which are more likely to be contracted when condoms or other barrier techniques are not used during sexual activity.
Douching may push dangerous germs into the reproductive organs and disturb the vagina’s normal bacterial balance, raising the risk of PID. Even though IUDs are typically safe, women who have an IUD implanted are somewhat more likely to develop PID in the initial weeks following insertion, particularly if they were already suffering from an undetected infection at the time of insertion.
The risk of this can be considerably decreased by being aware of these risk factors, using condoms, being tested for STIs often, and getting help right once symptoms appear.
Pelvic Inflammatory Disease Symptoms

- Abdominal Pain
From moderate and transient to more serious, many different illnesses can cause abdominal discomfort. The lower abdomen or pelvic region is frequently the site of abdominal pain in the context of Pelvic Inflammatory Disease (PID), although it can also radiate to the thighs or lower back.
This may also be connected to other illnesses such as urinary tract infections (UTIs), endometriosis, ovarian cysts, or appendicitis. You should contact a doctor for an assessment if your pain is severe or persistent, or if you have any of the other symptoms linked to PID. Early intervention can help avoid problems.
- Vaginal Discharge
A frequent sign of Pelvic Inflammatory Disease (PID) is vaginal discharge, which can differ in color, substance, and odor. An infection is typically indicated by an abnormal discharge when PID is present. The discharge may be thicker or more fluid than normal. The severity of the illness will determine whether it is more watery sticky or pus-like.
Getting medical help is crucial if the vaginal discharge changes color, odor, or consistency and is accompanied by additional symptoms such as pelvic discomfort, fever, difficulty urination, or pain during intercourse. These are indicators that an infection, such as PID, may be present and that antibiotics may be necessary to treat it.
Keep in mind that other illnesses can also produce irregular discharge, so it’s essential to have a good diagnosis to identify the source and provide the right medication.
- Painful Intercourse
Another typical sign of this is dyspareunia or painful sex. It may happen during or after intercourse and may indicate an infection or inflammation in the reproductive system. Infection and inflammation are brought on by PID in the ovaries, fallopian tubes, uterus, and other reproductive organs. The tissues may become sensitive and inflamed as a result of this inflammation, causing discomfort when the penetration occurs.
Seeking medical help is crucial if you have painful sex in addition to other PID symptoms. Antibiotics are a treatment option for PID, but if ignored, it can result in more severe side effects including infertility or persistent pelvic discomfort. Early treatment can help avoid long-term harm.
- Menstrual Bleeding
PID sufferers may have lighter or heavier-than-normal spotting or bleeding in between periods. This irregular bleeding occurs as a result of the infection’s potential to damage the uterine lining and interfere with the hormonal balance that governs menstruation. Some women have menstrual bleeding that is heavier than usual. The inflammation and discomfort brought on by the infection in the pelvic area are frequently associated with prolonged periods or increased flow.
Consult a healthcare professional if you encounter any unusual bleeding, particularly if it is accompanied by other symptoms such as pelvic discomfort, fever, painful sex, or abnormal vaginal discharge. The symptoms may indicate PID or another underlying illness that has to be treated.
Early diagnosis and treatment can help control these symptoms and avoid long-term issues including persistent pelvic discomfort or infertility.
- Difficulty Urinating
Dysuria, or painful urination, can be a sign of PID, particularly if the infection affects the pelvic organs or lower urinary tract. This discomfort is not always present, but it can be brought on by irritation and inflammation in the reproductive organs, which can spread to adjacent tissues like the urethra or bladder.
Seeking medical help is crucial if you have pain or trouble urinating in addition to other PID symptoms. Complications might arise from untreated PID, therefore it’s critical to have a correct diagnosis and treatment to prevent long-term problems.
- Fever and Chills
Fever and chills may be signs of an especially severe illness or that it has progressed outside of the reproductive organs. Therefore, if these symptoms appear, it’s imperative to get medical help, particularly if they’re accompanied by other PID symptoms like pelvic discomfort, unusual discharge, or painful sex.
You should get medical help right away if you have a fever, chills, unusual vaginal discharge, pelvic discomfort, difficulty urination, or pain during sexual activity. Fever can be a sign of a more serious or advanced infection that needs immediate treatment to avoid problems like infertility or persistent discomfort, especially when PID is present.
- Nausea and Vomiting
Because PID infects and inflames the reproductive systems, it can also impact the intestines and other surrounding organs, resulting in digestive symptoms including nausea and vomiting. These symptoms may be the result of a systemic reaction brought on by severe infection or pelvic abscesses (pockets of pus).
It’s critical to get medical attention right once if abdominal discomfort, fever, irregular vaginal discharge, or painful urination are present together with nausea and vomiting. To prevent problems like infertility, chronic pelvic discomfort, or damage to the reproductive organs, nausea and vomiting must be treated right away since they may indicate a more serious infection.
- Fatigue
Pelvic Inflammatory Disease (PID) is also frequently accompanied by fatigue, especially if the infection is more severe or has persisted for some time. The physical and psychological toll of enduring pain and discomfort may be the cause, or it may be the outcome of the body’s immune system exerting extra effort to fend off the infection.
An inability to fall asleep due to persistent pelvic pain, pain during sexual activity, or stomach discomfort can all lead to exhaustion. In addition to depleting your energy, chronic pain can make you feel more worn out all day.
It’s critical to get medical help if exhaustion is accompanied by additional symptoms such as pelvic discomfort, unusual discharge, fever, or trouble peeing. While fatigue on its own isn’t usually a warning indication, when combined with symptoms of PID, it may be a clue that the infection is hurting your general health and that you need to get help right away.
- Back Pain
The lower back’s nerves are linked to the pelvic regions. Inflammation or irritation in the pelvic area might cause the pain to “refer” to the lower back, giving the impression that the back, not the pelvis, is the source of the discomfort.
Seek medical attention if you have lower back discomfort in addition to other symptoms of PID, such as pelvic pain, fever, abnormal discharge, difficulty urine, or painful sex. Untreated PID can lead to serious consequences, therefore receiving antibiotics early on can help avoid long-term problems.
Back discomfort associated with PID usually gets better when the infection is treated, but treating the underlying cause is more crucial than treating the symptom. This can cause major side effects, such as infertility or persistent pelvic discomfort if treatment is not received.
PID (Pelvic Inflammatory Illness) and the Risk of Infertility
If treatment is not received, this may result in fallopian tube occlusion and permanent scarring. The fertilized egg cannot make it to the uterus through the fallopian tube, which might result in infertility.
You could be more likely to experience an ectopic pregnancy if you have had PID.
The following are some ways that PID may affect your fertility:
- You can treble your chance of tubal infertility with only one episode of PID.
- You have a 75% higher chance of fallopian tube obstruction if you have experienced three or more PID episodes.
- Ectopic pregnancy is seven times more likely to occur after one PID episode.
Identification of Pelvic Inflammatory Disease
See your doctor if you have any symptoms. A physical examination and tests for potential reasons will be performed by your physician.
A physical assessment of your pelvis to look for any swelling or soreness
- Tests on blood
- Test of urine
- Vaginal and cervical swabs
- Ultrasound
Sometimes a laparoscopy is necessary to properly diagnose PID. This process may involve the collection of a tissue sample.
Anesthesia is used to do laparoscopy. Your reproductive organs can be seen by inserting a thin tube with a tiny camera at the end into your belly button.
What Symptoms Of PID Are Most Prevalent?
Perhaps you are unaware that you have PID. Mild or undetectable symptoms are possible. PID symptoms, however, can also appear quickly. These may consist of:
- The most typical symptom is stomach or lower abdominal pain or soreness.
- Abnormal vaginal discharge, typically green or yellow, with a peculiar smell.
- Fever or chills.
- Nausea and vomiting.
- Suffering during intercourse.
- Urinating causes burning.
- Irregular cycles or experiencing cramps or spotting all month long.
Where Is The Discomfort From PID?
Your lower abdomen or pelvic area is where you feel the most discomfort from pelvic inflammatory diseases. It might have a subtle discomfort or feel sensitive and sore. Additionally, during intercourse, you could have profound pelvic discomfort.
The lower abdomen or pelvis are the most often reported sites of discomfort. Both continuous and sporadic, this pain can range from a dull aching to a severe, cramp-like agony.
One side of the lower abdomen may have more discomfort than the other, although the pain may also feel more widespread throughout the pelvic area.
Particularly if the infection has resulted in inflammation or pressure in the pelvic organs, discomfort may also radiate to the lower back. It might be more of a piercing pain or deep and painful.
When an infection affects neighboring tissues like the ovaries or fallopian tubes, it can sometimes cause pain or discomfort that radiates down to the thighs.
Although the most prevalent symptom of PID is pain, additional symptoms such as fever, nausea, exhaustion, and irregular vaginal discharge can also cause discomfort, making the whole experience of PID more unpleasant.
It’s critical to speak with a healthcare professional if you’re feeling uncomfortable in any of these locations, particularly if you’re also suffering other PID symptoms. Antibiotics can be used to treat PID, and early intervention can help avoid long-term issues.
What Causes Pelvic Inflammatory Disease?
This is caused by bacteria coming into contact with your reproductive system. These germs go up into your uterus, fallopian tubes, and ovaries from your vagina, via your cervix. When germs enter your vagina, they are normally prevented from moving further into other reproductive organs by your cervix. Infections of any kind, however, might interfere with your cervix’s ability to function.
This can be caused by a wide variety of bacteria, but the two most prevalent diseases that do so are chlamydia and gonorrhea. Unprotected intercourse is the source of both of these illnesses. About 90% of all PID cases are caused by these two STIs.
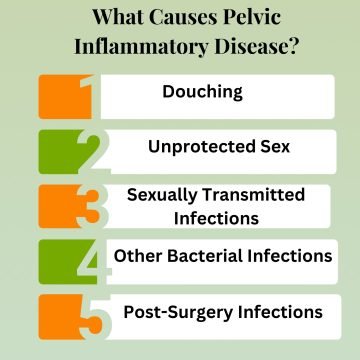
- Douching
Douching is the process of using water or a solution of water and other liquids to rinse or clean the vaginal interior. A specialized tool, such as a bottle or bag, is usually used for this, allowing the liquid to be released into the vaginal canal. Although douching is sometimes thought of as a means of vaginal cleanliness or odor removal, it can be detrimental and raise the risk of certain health issues.
The majority of gynecologists and medical specialists advice against douching since it can alter the normal vaginal environment and raise the risk of diseases like PID. Because the vagina is self-cleaning, cleanliness may typically be maintained by routinely bathing the exterior genital region with mild soap and water.
Instead of douching, it’s preferable to speak with a healthcare professional about any strange vaginal smells, discharge, or pain so that you can determine the source and get the right treatment.
- Unprotected Sex
Both gonorrhea and chlamydia, which are the most prevalent causes of PID, are spread via unprotected oral, anal, or vaginal intercourse. PID can result from these STIs infecting the cervix and then moving up into the uterus, fallopian tubes, and ovaries if treatment is not received.
During intercourse, the physical barrier created by condoms and other barrier methods of contraception lessens the spread of germs and viruses. Without this defense, you are more susceptible to infections, especially PID-causing ones.
Antibiotics can be used to treat many STIs, however, problems like PID can be avoided with early testing and treatment. For assessment and treatment, it’s critical to consult a healthcare professional right away if you experience symptoms like pelvic discomfort, unusual discharge, fever, or uncomfortable urination.
- Sexually Transmitted Infections
If gonorrhea-causing Neisseria gonorrhoeae bacteria travel from the cervix to the higher reproductive organs, it can also result in PID. Gonorrhea can be asymptomatic, similar to chlamydia, therefore many individuals may not be aware they have it until symptoms like PID appear.
This bacterial STI is less well-known but is becoming better recognized. It has been linked to PID. If left untreated, it frequently results in urethritis and cervicitis, which can progress to more severe infections of the reproductive system.
By upsetting the vagina’s normal bacterial balance and facilitating the ascent of pathogenic bacteria into the reproductive system, douching can raise the risk of infections, as was previously mentioned.
- Other Bacterial Infections
Bacterial overgrowth in the vagina, usually Gardner Ella vaginalis, is known as bacterial vaginosis. If the infection progresses to the higher reproductive organs, BV can raise the chance of getting PID even though it is not often regarded as an STI in and of itself. The vagina may become more vulnerable to STIs and other diseases as a result of BV.
The majority of PID-causing bacterial infections may be treated with medicines. Based on the kind of bacteria causing the infection, a specific antibiotic will be administered. Early treatment of PID is crucial to avoiding consequences like persistent pelvic discomfort or fallopian tube scarring.
- Post-Surgery Infections
There is a chance that germs might enter the body after any surgical treatment. Infections from microorganisms entering the uterus, fallopian tubes, or ovaries can result from pelvic or reproductive operations. The danger remains even when sterilization is done correctly.
A birth control method that is implanted inside the uterus is called an intrauterine device. A little chance of infection during or soon after the surgery exists, even though it is usually harmless. Infections that spread to the uterus and fallopian tubes after insertion might result in PID if germs are introduced into the reproductive system.
Long-term issues including infertility, persistent pelvic discomfort, or harm to the reproductive organs can be avoided with early diagnosis and treatment.
Identification of Male Pelvic Inflammatory Disease
In most cases, the physicians will suggest several diagnostic tests that aid in accurately assessing the condition and revealing its degree.
After doing an external physical verification, doctors will suggest imaging tests like CT, MRI, and ultrasound as well as blood and urine testing.
Men may also have bacterial infections that cause a similar kind of inflammation in their reproductive system, known as prostatitis or epididymitis. Although PID is a term used particularly to describe illnesses of the female reproductive organs, males can also have pelvic organ infections, usually as a result of untreated STIs or other bacterial infections.
Urethritis is an inflammation of the urethra that is frequently brought on by infections such as mycoplasma genitalium, chlamydia, or gonorrhea. Pelvic discomfort, discharge, and burning when urinating are some of the symptoms that may result from this. It is associated with reproductive tract infections, however, it is not PID.
Abscesses may develop in the reproductive organs in situations of severe infection, necessitating surgical drainage. A medical emergency known as sepsis can result from a serious infection that enters the circulation. Frequent STI examinations are crucial, particularly for people who engage in sexual activity and have several partners.
Therapy for Inflammatory Pelvic Disease
Antibiotics will probably be prescribed by your doctor to treat PID. Because your doctor might not be able to identify the exact type of bacteria that caused your infection, they may prescribe two separate medicines to treat different germs.
Your symptoms may get better or disappear a few days after you begin medication. Even if you feel better, you should still take your prescription to the end. The infection may reappear if you stop taking your medicine too soon.
Your doctor may refer you to the hospital for treatment if you are unwell or pregnant, have a pelvic abscess, or have trouble swallowing medicines.
Surgery may be necessary for this. Rarely, this is required only if a pelvic abscess ruptures or your doctor has reason to believe that one may. Additionally, it can be required if the infection doesn’t improve with treatment.
Sexual contact might transmit the PID-causing bacterium. If you engage in sexual activity, your partner should also receive PID treatment. Pelvic inflammatory disease-causing microorganisms may be silently carried by men.
If your spouse does not undergo treatment, your infection may return. You might be advised to refrain from having sex until the infection has been cleared up.
Strategies for Avoiding Pelvic Inflammatory Disease
- Having safe sexual behavior
- Undergoing testing for sexually transmitted diseases
- Staying away from jerks
- After using the restroom, wipe from front to back to prevent bacteria from getting into your vagina.
Options for Surgery to Treat Men’s Pelvic Pain
In certain cases, particularly if your pain is severe, the physicians may advise surgery. For the treatment of Pelvic Inflammatory Disease discomfort, this may now be advised, particularly if the problem is brought on by kidney stones, hernias, appendicitis, PVPS, or other conditions.
It’s important to keep in mind that doctors will only prescribe surgery if all other options, including medication and home treatments, have failed.
Surgery is usually reserved for extreme cases of pelvic floor dysfunction or persistent CPPS, in which the pelvic floor muscles become tense or unbalanced. But if physical therapy or muscle relaxants don’t work, surgeries can be utilized to fix pelvic floor problems.
In some situations of persistent testicular discomfort or pain originating from the testicles and epididymis that is not alleviated by previous therapies, orchiectomy may be advised, however, it is a more drastic alternative. If the discomfort is associated with persistent epididymitis, testicular malignancy, or testicular torsion, this is especially taken into account.
Male pelvic discomfort is often treated surgically only when no other treatment has worked and the source of the pain has been determined. The underlying problem causing the discomfort will determine which operation is best. To choose the best course of therapy, it is crucial to speak with an urologist or pelvic pain expert. Surgery should always be considered after less invasive treatments have been exhausted.
Do PID Complications Exist?
This might have increasingly severe effects the longer you have it. Your fallopian tubes may develop scar tissue as a result of the illness. Scarring can result in several issues, such as:
The most frequent consequence is chronic pelvic discomfort, which lasts for a long time. About 20% of adults, according to one research, experience persistent pelvic discomfort.
Scarring may stop a fertilized egg from entering your uterus, resulting in an ectopic pregnancy. Instead, it may implant inside your fallopian tubes as a result. Compared to those without PID, the rate of ectopic pregnancy is significantly greater in those with PID.
Up to 10% of individuals with PID have infertility as a result of scar tissue obstructing their fallopian tubes, which stops them from releasing an egg.
A tubo-ovarian abscess (TOA) is a pelvic infection pocket that can cause severe illness.
What Is The Impact Of PID On Fertility?
PID bacteria have the potential to leave scars on your fallopian tubes. An egg finds it more difficult to pass through this scar tissue from your ovary to your fallopian tube and ultimately to your uterus. To fertilize an egg, sperm must be able to pass through your fallopian tube.
The main location for fertilization is the fallopian tubes. PID may obstruct or damage the tubes, preventing the sperm from accessing the egg or the fertilized egg from reaching the uterus, if it results in scarring or damage to the tubes. One of the biggest effects of PID on fertility is this.
A woman with tubal infertility may have trouble becoming pregnant as a result of blocked tubes. If the fallopian tubes are significantly damaged or clogged, surgery may be necessary in extreme circumstances.
The implantation of a fertilized egg outside the uterus, typically in the fallopian tubes, results in an ectopic pregnancy. Ectopic pregnancies may become more likely if PID results in tube scarring.
If left untreated, ectopic pregnancies can result in rupture and internal bleeding, which can be fatal.
This can significantly affect fertility, especially if it is recurring or untreated. Important reproductive issues include adhesion development, fallopian tube damage, and an elevated chance of ectopic pregnancy. Effective therapy and early diagnosis, however, can help many women avoid long-term reproductive problems.
As you can see, several conditions, including kidney stones, appendicitis, urinary tract infections, and diseases involving the prostate glands, can cause men’s pelvic inflammatory disease. For short-term comfort, we have also suggested some natural solutions including the use of heating pads and medicines.
Ultimately, though, if these treatments prove ineffective, you might need to consult a doctor, take prescription medication, or have surgery. Through the Medypharmacy, you may also anonymously alert partners.