Introduction:
This is a problem that affects the pelvic muscles, causing them to become lacking in coordination. Whether you wish to control the need or have the want to urinate or defecate, your muscles would be unable to relax or contract.
This article will discuss the main causes of male pelvic floor dysfunction, identify some typical symptoms, and then examine several potential treatments to treat the condition.
Constipation, a need to urinate frequently, straining to defecate, and urine or stool leaks are some of the symptoms. Biofeedback, pelvic floor physical therapy, and medicine are among the treatments.
Male pelvic discomfort is a prevalent ailment that is often misunderstood and disregarded. The Pelvic Floor muscles form a sling-like structure at the base of the pelvis, supporting the pelvic organs, including the prostate gland, bladder, and rectum. Several symptoms might indicate male pelvic floor dysfunction when these muscles become weak, tense, or overactive.
Usually, these disorders arise from damage or gradual degradation of the pelvic muscles or connective tissue.
To understand pelvic floor dysfunction and its potential effects, it is essential to examine your pelvic floor’s basic anatomy and function.
These muscles control how much urine and feces you can produce. Keeping your pelvic organs safely and firmly inside your body is another important function of them.
Your ability to regulate your bowel and bladder movements may be affected if your pelvic floor muscles weaken. Women may also experience pelvic organ prolapse, a condition in which one of the pelvic organs shifts out of its normal position and loses support.
What is Male Pelvic Floor Dysfunction?
It is a frequent disorder in which you are unable to properly relax and coordinate your pelvic floor muscles to perform a bowel movement or pee. Imagine that your uterus, prostate, rectum, and bladder are all located in your pelvis. Your pelvic floor muscles serve as the foundation of your house. They are the framework that keeps everything in its proper position.
Your body contracts and relaxes your pelvic floor muscles, which allows you to use the restroom normally. Similar to clenching your fist or contracting your biceps when lifting a large box, this is a muscular activity.
But instead of releasing these muscles, your body continues to tense them if you have pelvic floor dysfunction.
- Having trouble passing a stool.
- Leaking of feces or urine.
This can also hurt when you’re having sex if you’re female. Males who experience erectile dysfunction may have trouble achieving or maintaining an erection.
- Bladder
- Rectum
- Urethra
- Uterus
- Vagina
- Prostate
Instead of letting your muscles rest, this makes you contract them. Consequently, you can have trouble passing gas.
This may cause pain, infection, or long-term colon damage if untreated.
Those who experience spasms or tight muscles may have problems passing feces or urinating. As they deteriorate, the pelvic organs may fall and pressure the bladder and rectum.
Comprehending Male Pelvic Floor Dysfunction
It is important to realize that the Pelvic Floor Dysfunction area in your home has several muscles and tissues that typically relax, making it simpler for stool or urine to exit.
Otherwise, in order to suppress such an urge, these muscular tissues would contract, obstructing the passage and emission of excrement or pee.
But the problem doesn’t occur until your body starts to lose control over certain muscle groups.
The problem with this is that the affected person is unable to regulate these muscular tissues.
You can either relax too soon, resulting in a sudden release, or the muscle tissues stay in contact even if you want to urinate or poop.
To control the urge to urinate or poop, the disorder involves losing control over the appropriate relaxing, squeezing, or stretching of these muscle tissues.
Exercises that relax or strengthen the pelvic muscles can be guided by a therapist. Biofeedback is frequently used in this process to assist patients better understand and manage their pelvic floor muscles.
This entails acknowledging the critical function of the pelvic muscles in maintaining bowel, sexual, and urine health. Chronic discomfort, incontinence, and sexual issues are just a few of the symptoms that can result from dysfunction in these muscles. Effective therapies are available to assist men recover control and enhance their quality of life, even if it may be an inconvenient or disregarded problem.
Types of Pelvic Floor Dysfunction
The primary classifications of pelvic floor dysfunction are dependent on whether the muscles of the Pelvic Floor are weak, prolapsed, excessively tight, or poorly coordinated. Sexual dysfunction, incontinence, and discomfort are just a few of the symptoms that these disorders can produce.
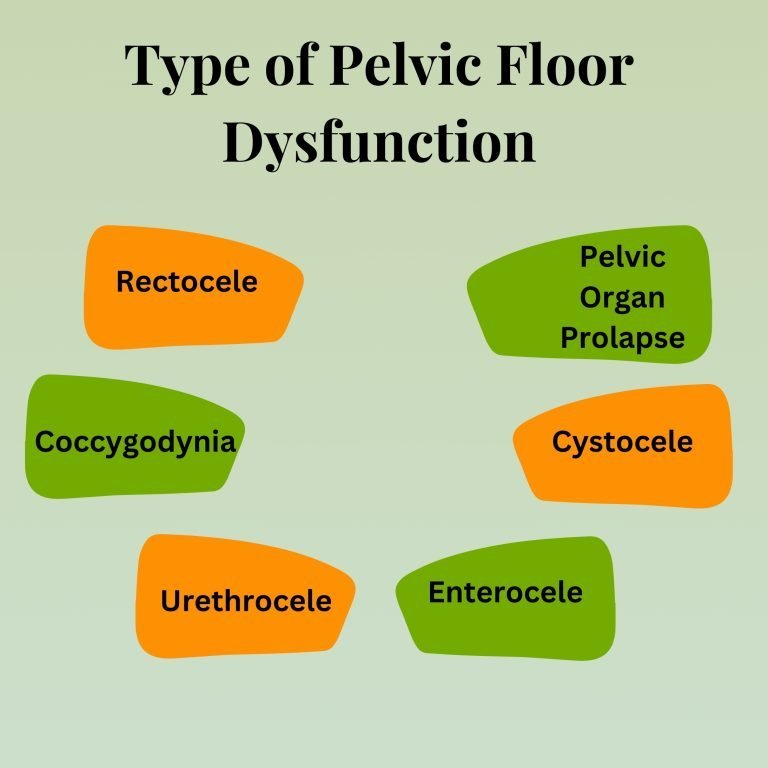
- Rectocele
A kind of pelvic organ prolapse (POP) known as a rectocele occurs when the rectum protrudes into the vaginal wall. When the pelvic floor’s muscles and tissues, which support the pelvic organs, weaken or strain, the rectum can drop and protrude into the vagina.
A rectocele is a form of pelvic organ prolapse that happens when the pelvic floor muscles weaken and the rectum protrudes into the vaginal wall. It may result in pelvic pressure, pain during sexual activity, and trouble with bowel movements, among other symptoms.
Depending on how bad the condition is, treatment options can vary from conservative approaches like pelvic floor exercises and dietary modifications to surgical repair. To find the best course of action if you think you may have a rectocele, it’s crucial to speak with a healthcare professional.
- Coccygodynia
The little, triangular coccyx bone, sometimes referred to as the tailbone, is located at the base of the spine and is the site of this pain. The bottom of the spine experiences localized pain or discomfort as a result of this ailment, which is usually made worse by sitting or specific motions.
A painful disorder affecting the tailbone, coccygodynia can be brought on by degenerative changes, repeated strain, trauma, or muscular tension. Usually, the symptoms include discomfort or pain near the base of the spine, particularly when sitting.
Conservative treatments, including sitting on padded surfaces, correcting posture, physical therapy, and medication, are frequently used. Surgery could be considered in extreme situations. Seeking medical help is crucial if you have tailbone pain to receive a proper diagnosis and treatment.
- Urethrocele
A kind of pelvic organ prolapse known as an urethrocele happens when the urethra protrudes into the vaginal wall. When the muscles and tissues that support the urethra weaken or stretch—usually as a result of childbirth, age, or increasing pelvic pressure—this ailment, which is more frequent in women, can develop.
A mesh may be used in certain situations to maintain the prolapsed urethra, however, this approach is being examined more closely because of the potential consequences. To support the pelvic organs and alleviate prolapse symptoms, a pessary is a device that is placed into the vagina. When surgery is either not desired or not soon required, pessaries are frequently employed.
- Enterocele
A kind of pelvic organ prolapse known as an enterocoele happens when the small intestine presses on the vaginal wall. This occurs when the muscles and tissues that support the uterus, bladder, rectum, and vagina weaken or stretch. Because of this, the small intestine, which is ordinarily located in the abdominal cavity, may protrude into the vaginal region, creating an enterocoele.
The pelvic floor muscles and tissues may strain or tear during vaginal delivery, which increases the chance of prolapse, particularly if there were difficulties like protracted labor, big infants, or repeated deliveries.
This deteriorates with age, increasing the risk of prolapse conditions. Because a decrease in estrogen can weaken pelvic tissues, this is particularly common in postmenopausal women.
Heavy lifting or chronic constipation are two examples of conditions that can put too much strain on the Pelvic Floor Dysfunction, pushing the small intestine against the vaginal wall.
- Cystocele
The bladder bulges into the vaginal wall in a cystocele, a kind of pelvic organ prolapse. The bladder and other pelvic organs are supported by the pelvic floor muscles and tissues, which can weaken or stretch. These tissues weaken, which permits the bladder to descend and results in a bulge in the vaginal wall. This can cause pain and other symptoms.
Prolapse risk can be increased by a decrease in estrogen levels, which can occur, for example, after menopause, and cause the pelvic floor tissues to become less elastic. Constipation-related straining during bowel motions can place a lot of strain on the Pelvic Floor, which can cause prolapse.
Some people may not have any symptoms at all, but more severe cystoceles can cause pelvic pressure, sexual discomfort, and urine incontinence. Pelvic floor exercises, pessary use, and, in more extreme situations, surgery to repair the prolapse are all possible forms of treatment.
- Pelvic Organ Prolapse
A disorder known as pelvic organ prolapse (POP) occurs when one or more of the pelvic organs protrude into or out of the vaginal canal after slipping from their natural place. This happens when these organs’ supporting muscles, ligaments, and connective tissues deteriorate or weaken. Numerous symptoms, such as pelvic discomfort, urinary problems, and vaginal bulging, might be brought on by the prolapsed organs.
In order to keep the pelvic tissues strong and flexible, estrogen is necessary. Lower estrogen levels during menopause may be a factor in the development of pelvic organ prolapse. Chronic coughing can put strain on the Pelvic Floor and raise intra-abdominal pressure, especially if it is brought on by smoking, asthma, or chronic bronchitis.
When Dealing With Male Pelvic Floor Dysfunction, You May Notice Some Symptoms.
Now, let’s learn about some of the typical signs that indicate that you could be experiencing male pelvic floor dysfunction problems.
- Recurring need to urinate
- Starting the flow of pee is difficult
- Poor flow of urine
- Using self-control to initiate the urine flow
- Following a urination, dribbling
- The inability to pass stool
- There are instances when straining to pass feces produces excruciating agony.
- Being constipated
- Leaking of stool
- Back discomfort in the lower back
As you can see, identifying and evaluating the symptoms would not be too difficult. Simply check to see if you frequently experience any of these symptoms when you urinate or poop.
See a physician for an appropriate remedy and treatment to stop the disorder from worsening.
Diagnosis for Pelvic Floor Dysfunction
You will be questioned about your health by your physician. This will entail learning about your bowel movements, past UTIs, and any additional illnesses that may contribute to Pelvic Floor Dysfunction. If you’re a woman, your doctor could inquire about your history of pregnancy and whether you have pain during intercourse.
Both an exterior and internal examination may be performed by your physician to assess the health of your muscles. To assess the function of your pelvic floor muscles, further tests are available.
- Putting electrodes on your pelvic region’s surface to gauge how well your muscles work.
- Measuring the effectiveness of the anal sphincter by doing an anal manometry. In this procedure, a thin, flexible catheter is passed into your anus and has an uninflated balloon attached to the end. As it is gradually removed several times, it enters your rectum and records pressure changes.
- Delivering a defecating proctogram, a test in which your doctor will watch how your muscles contract to push out a thick enema by showing it on an x-ray.
- To demonstrate how well your bladder empties each time you urinate, do a uroflow test.
What Causes Pelvic Floor Dysfunction?
- Age
- Systemic Diseases
- Lasting Health Issues
- Pregnancy
- Trauma During Delivery
- Multiple Deliveries
- Large Babies
- Operative Delivery
Research shows that around half of all postpartum women experience either pelvic organ prolapse, stress urine incontinence, or both. Injury to the pelvic floor muscles after delivery is intimately linked to these problems.
Urinary incontinence may be classified into many categories.
With aging, the pelvic floor muscles can also naturally stretch. As women age, for instance, stress urine incontinence and pelvic organ prolapse become increasingly prevalent.
The capacity of the muscles to support the pelvic organs might also be impacted by collagen diseases.
Meanwhile, trauma to the tailbone, such a fall, is typically the cause of coccygodynia. In around one-third of cases, however, the cause of coccygodynia is not identified. Experiencing discomfort may make bowel movements challenging.
Several elements contribute to this complicated illness. Childbirth, aging, hormone fluctuations, obesity, prolonged straining, trauma or injury, nerve damage, and certain medical diseases are regular causes. A lot of these issues are connected, and pelvic floor dysfunction is frequently caused by many circumstances.
To successfully prevent or treat pelvic floor dysfunction, people can identify and address risk factors such as weak pelvic floor muscles, bad posture, and excessive straining.
For an appropriate assessment and treatment plan catered to your requirements, it is crucial to speak with a healthcare professional if you are dealing with symptoms such as pelvic pressure, painful sex, urine incontinence, or trouble passing stool.
How Do You Treat Pelvic Floor Dysfunction?
To improve control and facilitate bowel movements, the treatment aims to relax the pelvic floor muscles.
Exercises that force you to contract your muscles, such as Kegel exercises, won’t assist with this issue. There are less intrusive treatment alternatives available, even though surgery is a possibility.
Biofeedback is a popular therapy for this illness. With this method, your therapist can use specialized sensors to track how you contract or relax your pelvic muscles. Following an assessment of your muscle activity, your therapist will provide you with guidance on how to enhance your coordination.
- Medications
This results from stiffness or spasms in the pelvic floor muscles; to relieve this tension, doctors may prescribe drugs such as muscle relaxants.
Topical estrogen reduces vaginal dryness and enhances muscular function in postmenopausal women by increasing the flexibility and strength of pelvic floor tissues.
This can be treated with prescription painkillers or over-the-counter drugs like ibuprofen
When an overactive bladder is linked to pelvic floor dysfunction, it can be utilized to treat bladder symptoms, including urgency and frequency.
- Pessaries
To support the pelvic organs and reduce prolapse symptoms, a pessary is a device that is placed into the vagina. For ailments like vaginal or uterine prolapse, pessaries are frequently utilized and can be a successful non-surgical treatment.
To prevent or lessen prolapse and assist in managing incontinence, a pessary mechanically supports the pelvic organs and vaginal walls. Long-term use is possible, but it must be closely watched for hygiene and fit issues.
- Sexual Therapy
It may be advised for those with pelvic floor dysfunction that impacts sexual function to consult a pelvic floor physical therapist or a sexual therapist. This includes those who have painful intercourse or loss of sensation.
Couples’ communication tactics and methods to ease pelvic floor muscle tension and promote relaxation may be part of therapy.
- Surgical Treatments
Surgical procedures could be taken into consideration if conservative therapy is ineffective or if the pelvic floor dysfunction is severe. These operations are usually only performed when symptoms substantially impair day-to-day functioning or quality of life.
To give the pelvic organs long-term stability, the vaginal walls are attached to the sacrum. For vaginal or uterine prolapse, it is frequently utilized.
When the Pelvic Floor Dysfunction is too weak to regulate pee during activities like coughing, sneezing, or exercising, stress urinary incontinence is treated surgically.
Sometimes pelvic floor dysfunction causes bladder incontinence, which can be treated with surgery that raises and supports the bladder.
- Electrical Stimulation
The strength and coordination of the pelvic floor muscles are enhanced by electrical stimulation. To assist the pelvic muscles in contracting and strengthening, tiny electrical impulses are sent to them. A vaginal or rectal probe, or pads applied externally to the skin, can be used for this procedure.
Sacral Nerve Stimulation: Electrical impulses are sometimes sent to the sacral nerve to help regulate bladder function and reduce incontinence symptoms.
- Cognitive Therapy
People with pelvic floor dysfunction who suffer from emotional discomfort, anxiety, or depression may find that Cognitive Behavioral Therapy (CBT) helps. It can enhance people’s general well-being and assist them in managing their symptoms.
These can improve function and lessen discomfort by relaxing the pelvic floor muscles in those who have pelvic pain or muscular tension.
- Pelvic floor physical therapy
One of the most popular and successful treatments for pelvic floor dysfunction is conducting specific exercises to strengthen the pelvic floor muscles. Kegel exercises aid in prolapse treatment, incontinence reduction, and muscle tone improvement.
Kegel exercises include the contraction and relaxation of the muscles involved in sexual function, bowel motions, and urine. To learn how to perform these exercises properly, consult a pelvic health physical therapist.
This method helps people become more conscious of the way their pelvic floor muscles are working. Muscle contractions are tracked by sensors applied to the body, which provide real-time input to enhance muscle control.
To relieve muscular spasms, relax tight pelvic muscles, and enhance pelvic floor function, a pelvic floor physical therapist may employ manual treatments.
To lessen pelvic floor tension and stop symptoms from becoming worse, teach good posture, body mechanics, and relaxation methods.
- Lifestyle Modifications
Reducing straining during bowel movements and increasing dietary fiber and fluid consumption might help ease pressure on the pelvic floor if constipation is causing pelvic floor dysfunction.
By keeping a healthy weight, prolapse and incontinence symptoms can be alleviated by lowering the strain on the Pelvic Floor Dysfunction.
Bladder training methods can help retrain the bladder to retain pee for longer periods and with less urgency in those who have urinary incontinence.
Limiting exercises that overstress the pelvic floor, such as heavy lifting, can cause more harm and alleviate symptoms.
Is Your Pelvic Floor Able To Be Restored?
It can take several months of physical therapy sessions before you see any relief in your symptoms. But ultimately, most individuals do see a difference. For more than 75% of individuals with pelvic floor dysfunction, biofeedback improves muscular control.
The degree to which the Pelvic Floor Dysfunction may be recovered varies based on the underlying reasons, the degree of dysfunction, and the particular therapeutic strategy. Enhancing tissue health, retraining and strengthening the muscles, and treating any underlying causes are all common components of pelvic floor therapy. Even while restoration doesn’t necessarily include going back to how things were before the dysfunction, with the correct care, major progress may frequently be made.
By releasing tense or hyperactive pelvic muscles, this hands-on therapy can enhance muscular balance and reduce discomfort.
You can manage your bowel and bladder habits to lessen the strain on your pelvic floor with the help of a pelvic floor physical therapist.
If this is properly treated, it may often be much improved or even completely recovered. Complete restoration, however, is contingent upon the underlying cause, degree of severity, and responsiveness to therapy. While lifestyle modifications and pelvic floor therapy may frequently completely cure mild to moderate dysfunction, more severe instances may require a combination of therapies, including surgery.
In What Ways Do I Look After Myself?
The key to coping with this is never to give up. Regular pelvic floor physical therapy and bowel or urine drugs may be necessary for several months before symptoms begin to improve. However, most patients who follow their treatment plan report feeling better.
Keep your therapy sessions and medication appointments. Your symptoms may worsen and persist if you forget to take your medication. Healing might also be slowed by missing physical therapy sessions or not doing exercises.
Avoid doing anything that makes your pelvic floor more tense or painful. Any activity with this effect has the potential to exacerbate your symptoms. For instance, jumping repeatedly or lifting large weights can exacerbate pelvic floor tension and its symptoms. Take note of your body. For advice on which activities to avoid, speak with your healthcare provider or physical therapist.
As you follow a healthy diet, make sure to stay hydrated. Constipation can be avoided by consuming more than eight glasses of water each day. Consume foods that don’t produce uncomfortable side effects. High-fiber foods or supplements, for instance, may exacerbate gas pains or bloating symptoms. Steer clear of them if your symptoms get worse. Your healthcare professional can suggest wholesome foods that aren’t uncomfortable.
Methods for Treating Male Pelvic Floor Dysfunction
We will learn about potential strategies for overcoming this illness in this final section before we wrap up our article.

- Pelvic Floor Exercises
Doing pelvic floor exercises more frequently is one of the natural solutions for male Pelvic Floor Dysfunction.
Exercises include stretching, compression, squeezing, and relaxation of the pelvic muscles, which may improve voluntary movement and control of these tissues while also increasing blood flow.
You can get assistance from a physiotherapist to perform these sets of exercises.
- Biofeedback
In order to better understand and assess how you can properly regulate your pelvic floor muscles, the physicians will use movies, sensors, and other visual technologies to observe your pelvic floor muscle contractions and movements.
Once they have finished their study, which will involve reviewing the movies and tracking sensor data, they will assist you in giving this input.
- Acupuncture Therapy
Acupuncture treatment from professionals is one potential treatment for male pelvic floor dysfunction. Using pricking needles to improve blood flow to the pelvic muscle tissues and raise local sensitivity may help improve control over these muscle tissues in this type of traditional medicine.
- Water Bath
The doctors would advise you to take a warm water bath or hot water bath every day to induce better blood flow to the muscles and relax the pelvic region’s muscle tissues.
Treatments Using Stem Cells
A 2016 study’s researchers looked at whether a stem cell-based treatment may help rats with pelvic floor dysfunction.
The stem cells were put into rats with pelvic floor dysfunction after the researchers modified them to make and release collagen and elastin into the pelvic floor.
Stress urine incontinence symptoms were reduced, and pelvic floor components were repaired, thanks to the collagen and elastin.
In the latter part of the investigation, the scientists created stem cells that inhibited a factor that prevents elastin from being produced. This encouraged more elastin to be produced and released into the Pelvic Floor.
Additional studies may reveal that comparable treatments work well for people.
As you can see, the main difficulty that men have that can lead to a lot of issues while urinating and defecating is pelvic floor dysfunction.
We have provided you with information on the symptoms so that you can easily identify them and seek medical attention as soon as they appear.
Consulting a professional will be crucial if you have pelvic floor issues. Medypharmacy is a senior physiotherapist with a focus on pelvic therapy at the facility.